New Birmingham Implant Retrievals Centre set to advance patient safety through understanding of implant failure
A new research partnership led by Birmingham Health Partners members the University of Birmingham and the Royal Orthopaedic Hospital NHS Foundation Trust (ROH) will formally launch on Monday 23 March, bringing together clinicians, engineers, regulators and industry to improve understanding of joint implant performance and failure.
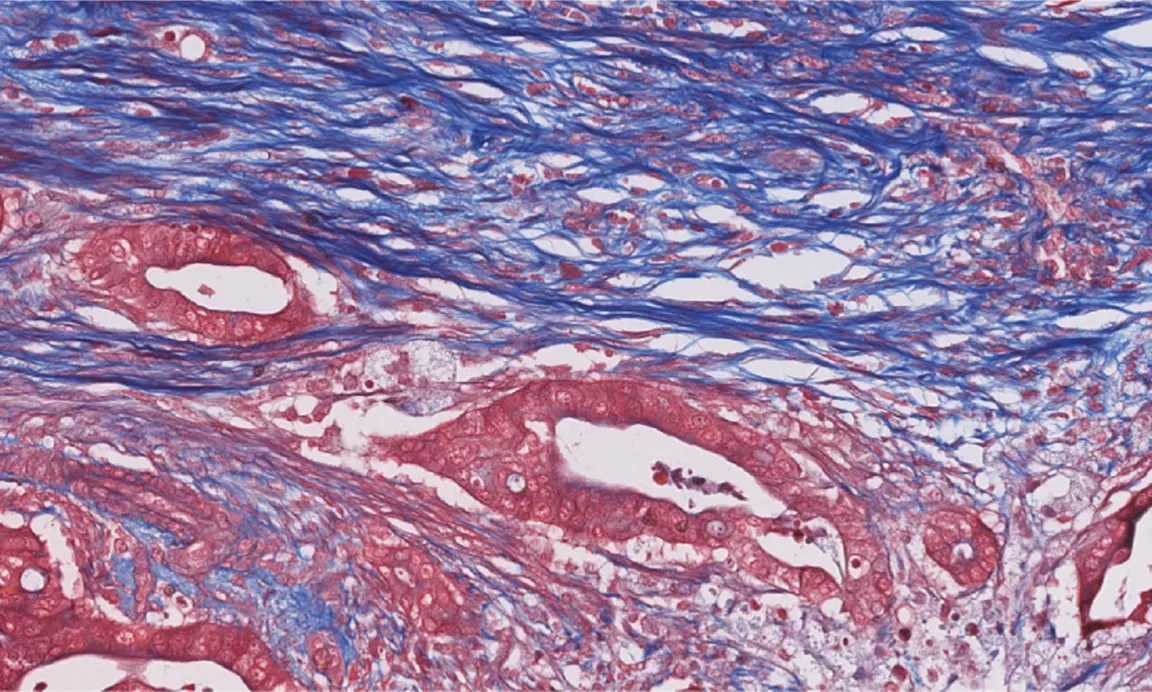
Concerns around implant performance – particularly metal-on-metal joint replacements – have highlighted the need for robust evidence on implant behaviour. The Birmingham Implant Retrievals Centre will focus on analysing retrieved orthopaedic implants and associated tissue samples to identify why devices fail, how implants behave inside the body, and how patient safety can be improved through earlier identification of risk.
The University of Birmingham leads the centre in collaboration with Birmingham Health Partners, with ROH as the primary clinical partner. Additional partners include the Medicines and Healthcare products Regulatory Agency (MHRA), the US Food and Drug Administration (FDA), ODEP, Beyond Compliance, and industry collaborators.
University of Birmingham researchers are applying advanced engineering expertise to the study of retrieved implants, working closely with surgeons at ROH to understand how devices perform over time in patients. ROH is one of the UK’s largest centres for revision surgery and a global leader in orthopaedic oncology, providing access to a significant volume of patient data associated with revision procedures.
By coordinating retrieval, consent, and transfer processes between ROH and the University, implants and tissue samples can be analysed quickly using a comprehensive engineering pipeline including photography, microscopy, metrology and materials characterisation. This enables detailed insight into wear, corrosion, material degradation and failure mechanisms. The linkages with clinical data and close working relationships with clinicians, regulators and industry ensure actionable insight, closing the loop on implant life-cycle and future development.
The centre aims to answer critical questions including:
- What trends exist in implant failure including surgeries that would be otherwise low-volume numbers at other UK hospitals – for example limb salvage)?
- Why do failures occur?
- What does a mechanically well-functioning joint look like
- How can earlier identification of risk improve patient safety?
A key feature of the centre is its embedded infrastructure within ROH, which enables the routine collection of explanted devices and associated clinical data without requiring clinicians to do anything beyond their usual standard of care.
Expected outcomes include enhanced patient safety through earlier detection of failure risk, improved understanding of revision arthroplasty drivers, and evidence to support better screening and testing of both new and existing implant devices. Findings will feed into early warning systems and support compliance with guidance from organisations including NICE, MHRA, FDA, and ODEP.
Professor Michael Bryant, Professor of Tribology and Corrosion Engineering at the University of Birmingham, said: “We are delighted to partner with the Royal Orthopaedic Hospital on this important initiative. Routine explant analysis, robustly linked to clinical records and National Joint Registry data, is a vital component of evidence-based life-cycle evaluation for both established and emerging orthopaedic devices. Explant analysis has long been, and continues to be, a key tool for detecting potential device-related safety signals and root cause failure mechanisms, strengthening post-market surveillance, and ultimately enhancing patient safety.”
Professor Adrian Gardner, Research and Development Director and Consultant Spinal Surgeon at the Royal Orthopaedic Hospital, said: “While joint replacement implants – and therefore patient outcomes – have improved significantly, understanding why these implants fail is critical. We’re thrilled to be partnering with the University of Birmingham to bring this research to the Midlands, supporting local researchers with this essential work that will ultimately improve patient safety through the enhanced performance of joint replacement devices.”
Dr Andrew Robert Beadling, Assistant Professor in Biomedical Engineering at the University of Birmingham said: “Preclinical assessment for joint replacements and MSK implants relies on simplified, idealised conditions to determine artificial ‘benchmarks’ of performance. Because this testing doesn’t represent real-world conditions, it provides limited actionable information and is often unrelatable to clinical outcomes. The Birmingham Implant Retrieval Centre enables the study of retrieved implants so we can better design preclinical testing according to how devices fail in the field, improving patient safety.”
This work follows longstanding recommendations to improve monitoring of implant safety and outcomes. The partnership also represents a further formalisation of research collaboration between the University of Birmingham and the Royal Orthopaedic Hospital, strengthening translational research links between engineering and clinical practice.
The Birmingham Implant Retrievals Centre partnership will be officially launched with a kick-off meeting at the Royal Orthopaedic Hospital on Monday 23 March.