The BHP Starter Fellowship – Joseph’s story
The BHP Starter Fellowship – Joseph’s story
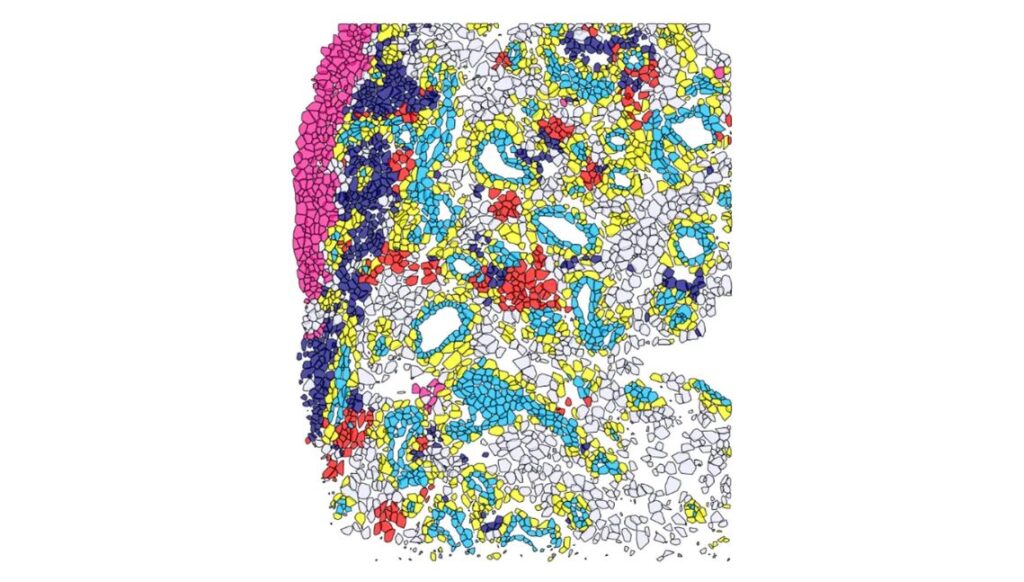
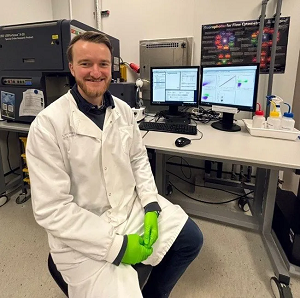 Dr Joseph Sturman is a a Kidney Research UK (KRUK) Clinical PhD Fellow investigating how Chronic Kidney Disease (CKD) leads to altered immunometabolism and increased susceptibility to infectious diseases. Ultimately, his aim is to understand how we can modulate immunometabolism to improve the control of infectious diseases in this vulnerable population, using Mycobacterium tuberculosis (Mtb) as a model pathogen. His PhD funding application to KRUK was successful thanks to the excellent supervisory support and fundamental preliminary data he collected during his BHP Starter Fellowship in 2023 – 2024.
Dr Joseph Sturman is a a Kidney Research UK (KRUK) Clinical PhD Fellow investigating how Chronic Kidney Disease (CKD) leads to altered immunometabolism and increased susceptibility to infectious diseases. Ultimately, his aim is to understand how we can modulate immunometabolism to improve the control of infectious diseases in this vulnerable population, using Mycobacterium tuberculosis (Mtb) as a model pathogen. His PhD funding application to KRUK was successful thanks to the excellent supervisory support and fundamental preliminary data he collected during his BHP Starter Fellowship in 2023 – 2024.
What attracted you to apply for the BHP Starter Fellowship?
I knew I wanted to be actively involved in research after enjoying my intercalated degree in biomedical sciences, but I wanted to focus on acquiring my clinical competencies when I first graduated from medical school. Once I obtained my specialty training number in renal medicine, I decided it was a good time to explore research again, and the BHP Starter Fellowship offered an ideal opportunity to pursue these interests.
What were the benefits of the fellowship?
The BHP Starter Fellowship offered the protected time and opportunities to participate in meaningful research which would otherwise not be possible for a full-time clinical trainee like myself who did not have the privileges of an academic clinical fellowship earlier in their career. The fellowship was therefore an essential springboard for launching my academic career and I am hugely grateful for the opportunity.
Were there any challenges during the fellowship?
The main challenge was the very steep learning curve to acquire new laboratory, bioinformatic and statistical analysis skills rapidly in order to produce meaningful outcomes within 12 months. Nevertheless, the fellowship was extremely well supported, and the supervision was excellent which meant meeting this challenge was achievable and enjoyable.
How much clinical work did you do while undertaking your fellowship?
During my 12-month fellowship, I did not undertake any clinical work. With so many research skills to acquire, I am glad that I took the time away from clinical commitments as the fellowship was a unique opportunity to gain skills that I wouldn’t get again. Re-entering clinical work after 12 months was challenging but also well supported. Now I have acquired essential research skills, I feel more comfortable undertaking some clinical commitments to ensure I do not lose my clinical skills during my PhD. I currently contribute ~20% of my time to the on-call renal registrar rota while undertaking my PhD.
Did the fellowship help with your clinical practice?
I think the fellowship has helped me become a more well-rounded doctor by developing my analytical and decision-making skills. It has also opened opportunities to write reviews on clinical conditions and case reports which has directly furthered my clinical knowledge base.
Do you feel that the fellowship has helped you with your career development and aspirations?
Absolutely! The fellowship has been essential to my career development and I am in no doubt that without it, I would not have been able to embark on a PhD. The fellowship has opened up so many opportunities for collaboration and research both locally and nationally, and I look back on the BHP Starter Fellowship as a pivotal moment in my career.
What would your advice be to anyone thinking of applying for a BHP fellowship?
This is a golden opportunity for anyone who wants to be involved with research but hasn’t completed an academic clinical fellow job earlier in their training. I advise contacting potential supervisors at least a year before applying to give you time to work on a project idea and to get your CV in the best possible shape. To be successful, you need to be able to demonstrate a clear commitment to research, and a cohesive project plan with supervisors who are willing to support you, so give yourself time to work on this. I started by approaching potential supervisors, who gave me some small projects to help me demonstrate my commitment to research, and the project plan came together in discussion with them. All this takes time so start thinking about this early.
 Dr Mark Openshaw is a Consultant Medical Oncologist at BHP founding member University Hospitals Birmingham NHS Foundation Trust. His
Dr Mark Openshaw is a Consultant Medical Oncologist at BHP founding member University Hospitals Birmingham NHS Foundation Trust. His 



 Dr Anna Seale is Paediatric Consultant at Birmingham Children’s Hospital, part of BHP founder-member Birmingham Women’s and Children’s NHS Foundation Trust. Through her BHP
Dr Anna Seale is Paediatric Consultant at Birmingham Children’s Hospital, part of BHP founder-member Birmingham Women’s and Children’s NHS Foundation Trust. Through her BHP