Integrated clinic pilot shows potential to cut costs while improving care for children in deprived areas
New research suggests that integrating health and early years support could ease pressure on NHS services while delivering better outcomes for families.
Undertaken by the Birmingham Health Partners (BHP) Evaluation Service, a detailed assessment of the Sparkbrook Children’s Zone (SCZ) in Birmingham found indications that integrating health care with early years and family support in deprived communities may be a cost-effective alternative to standard primary care.
The model-based economic analysis shows that children and young people accessing the SCZ clinic were less likely to attend A&E and require social care support compared to those receiving standard care, with an average cost saving per patient of £44 – achieved mainly by reducing referrals to children’s social care and emergency health services.
Sparkbrook, one of Birmingham’s most deprived neighbourhoods, is the first area to pilot this joined-up approach. The clinic brings together primary care, early years services, and family support under one roof, aiming to provide more holistic and preventative care.
Dr Mark Monahan, Lecturer in Health Economics at the University of Birmingham, explained: “Rising rates of child poverty, mental health issues and emergency hospital use show that our current systems aren’t working well enough for children and families in deprived areas. This pilot shows real promise in delivering better outcomes at lower cost, but we urgently need further evaluation to build the evidence base.”
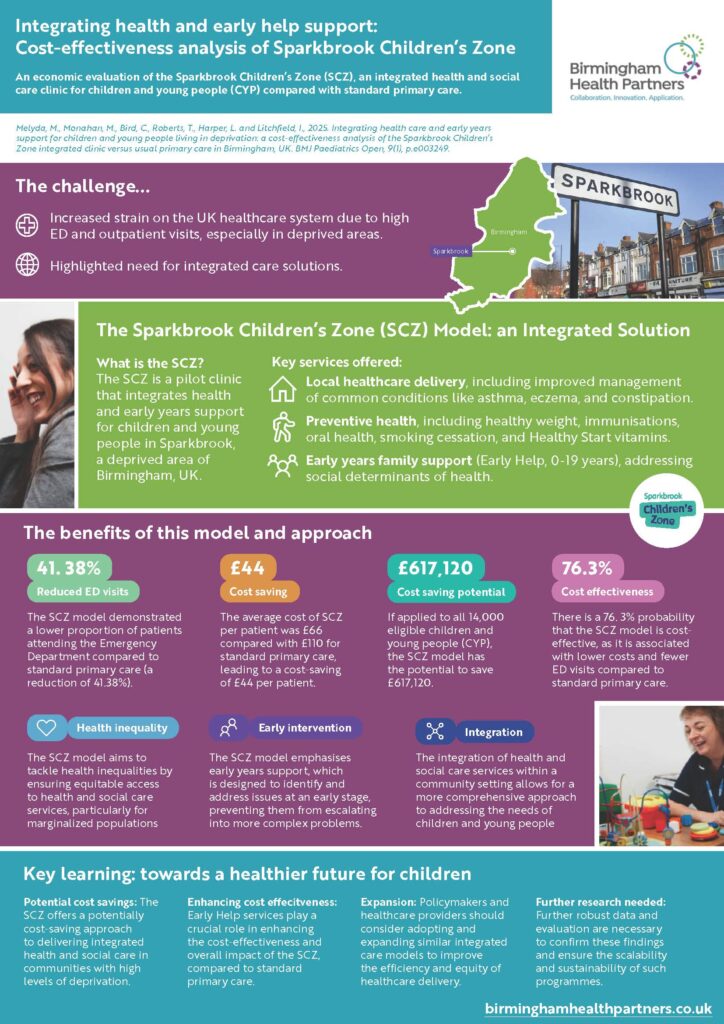
The analysis showed a lower proportion of emergency department visits among SCZ patients (1.7%) compared to those in standard primary care (2.9%), driven by earlier intervention and integrated support, with SCZ patients were 40% less likely to attend A&E than those in standard care. This reduced reliance on emergency and social care services translated into significant potential savings, even with the limited data currently available. Early Help services embedded in the clinic were a key driver of cost-effectiveness by addressing complex family needs earlier.
While these findings are based on preliminary modelling, the results support NHS England’s ambition to develop more community-based, joined-up care models for children and young people.
The study also highlights the need for more robust and long-term data to support the national roll-out of similar models. It calls on policymakers, researchers and practitioners to work together to address evidence gaps and ensure these innovations are scalable, sustainable and capable of tackling entrenched health inequalities.
The Birmingham Health Partners Evaluation Service was established in 2022 to provide time-sensitive, formative evidence on innovations in healthcare and capacity building. It carries out rapid and effective service evaluations, often running in parallel with service implementation; helps spread learning to other sites; and helps build local capacity for in-house evaluations.

 Dr Anna Seale is Paediatric Consultant at Birmingham Children’s Hospital, part of BHP founder-member Birmingham Women’s and Children’s NHS Foundation Trust. Through her BHP
Dr Anna Seale is Paediatric Consultant at Birmingham Children’s Hospital, part of BHP founder-member Birmingham Women’s and Children’s NHS Foundation Trust. Through her BHP



