New vaccine trial for head and neck cancer patients
Patients in Birmingham who have advanced head and neck cancers may be eligible to take part in a new clinical trial of a potential cancer vaccine, supported by the NHS Cancer Vaccine Launch Pad (CVLP).
Queen Elizabeth Hospital Birmingham, part of BHP founder-members University Hospitals Birmingham NHS Foundation Trust (UHB), is one of 15 sites across the country aiming to recruit more than 100 patients over the next year.
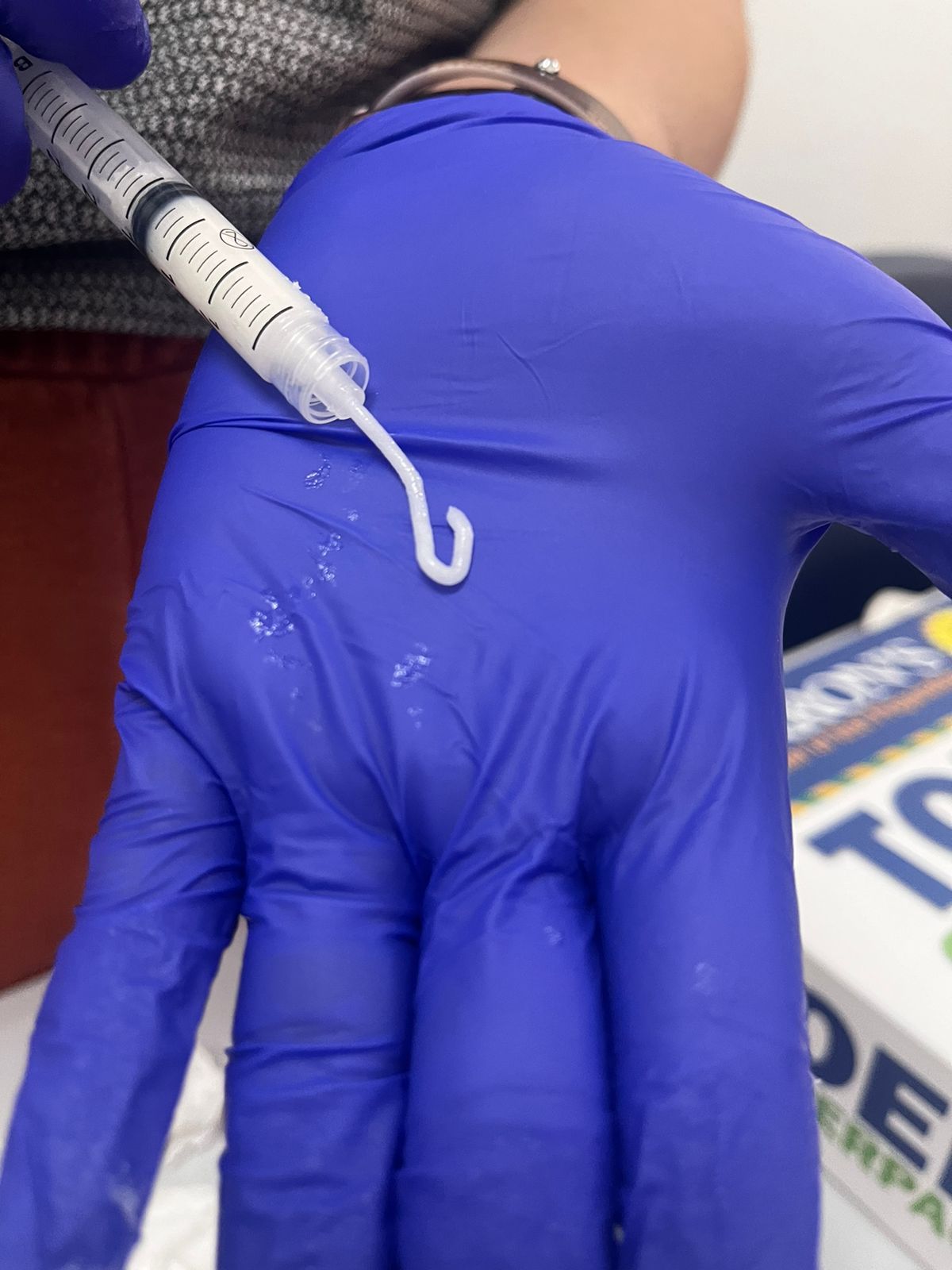
The investigational cancer vaccine in this latest trial on the platform uses mRNA technology to help the immune system recognise and kill cancer cells which express human papillomavirus (HPV) proteins.
The first head and neck cancer patients in England have received the investigational mRNA cancer vaccine in the clinical trial, known as AHEAD-MERIT (BNT113-01), with more patients to soon be enrolled at their nearest NHS hospital.
More than 11,000 new head and neck cancer cases are diagnosed in England every year, with cancers typically developing in the mouth, throat or voice box.
Despite advances in care for patients with head and neck cancer, the advanced form of the disease is difficult to treat and has high rates of recurrence, with two-year survival rates at under 50%.
The investigational cancer vaccine is designed to encode two proteins that are frequently found in head and neck squamous cell cancers associated with human papillomavirus (HPV-16). This is the most common type of head and neck cancer, accounting for 95% of these types of cancers, and the vaccine aims to train the immune system to fight the cancer.
NHS England is partnering with life sciences company BioNTech to help identify potentially eligible patients to refer to NHS hospitals running the clinical trial.
Dr Paul Sanghera, Consultant Oncologist and Principal Investigator of the trial at Queen Elizabeth Hospital Birmingham, said: “This clinical trial marks an important step forward in the search for better treatments for advanced head and neck cancers, which remain a significant challenge in oncology.
“These cancers are notoriously difficult to treat, and access to this investigational vaccine could offer patients a potential new option in their treatment journey. While we are still in the early stages, the hope is that this trial will pave the way for improved outcomes for those living with these challenging conditions.”
Matthew Metcalfe, Hospital Executive Director at Queen Elizabeth Hospital Birmingham, said: “We are incredibly proud to be one of the 15 sites across the country taking part in this important clinical trial. It reflects our ongoing commitment to driving forward research aimed at improving outcomes for patients in Birmingham and beyond, offering new hope to those facing these challenging diagnoses.”
Dr Iain Foulkes, Executive Director of Research and Innovation at Cancer Research UK, said: “It’s great to see more clinical trials of vaccines for head and neck cancer supported by the Cancer Research UK-funded Southampton Clinical Trials Unit.
“Research into personalised cancer treatments is vital. There are over 200 different types of cancer and it’s unlikely there will ever be a single cure that works for everyone. That’s why it’s vital that we support a wide range of research, so that more people can live longer, better lives, free from the fear of cancer.”