NIHR awards £4m to Birmingham Clinical Research Facility to enhance the delivery of research
The Birmingham NIHR Clinical Research Facility (CRF) has been awarded £4 million from the National Institute for Health and Care Research (NIHR).
This funding is part of a total investment of £96 million that has been awarded to NHS organisations across England, to enhance the delivery of research through improving research facilities for patients across the NHS, helping teams to find new ways to prevent and treat diseases.
The Birmingham NIHR CRF is a collaboration between three BHP members – University Hospitals Birmingham NHS Foundation Trust (UHB), Birmingham Women’s and Children’s NHS Foundation Trust (BWC) and the University of Birmingham (UoB).
In Birmingham, new equipment will enable the delivery of innovative health technology services, including a range of cell and gene therapies requiring specialist pharmacy facilities. For example, onsite isolators will support preparation within the research facilities, speeding up the delivery of CAR-T trials for patients with haematology (blood) cancers, as well as trials into cancer vaccines for patients with a variety of solid tumour cancers.
The funding will also provide new laboratory equipment, essential for storing samples from patients recruited to metabolic research studies. This will support researchers with ground breaking work in the prevention, treatment and management of metabolic disease for adults and children across Birmingham.
The bid was led by Jo Gray, NIHR Birmingham Clinical Research Facility Clinical Manager, who said: “This successful bid for equipment and upgrades to our facility is fantastic and will make such a difference to patients and research teams across all partner sites.
“We have ambitious plans in place to upgrade existing equipment, as well as increase our ability to support new research across the sites. New equipment will include a paediatric ‘peapod’, which measures body composition and growth in premature born infants, and biosafety cabinets, which provide an enclosed ventilated space for drug preparation.
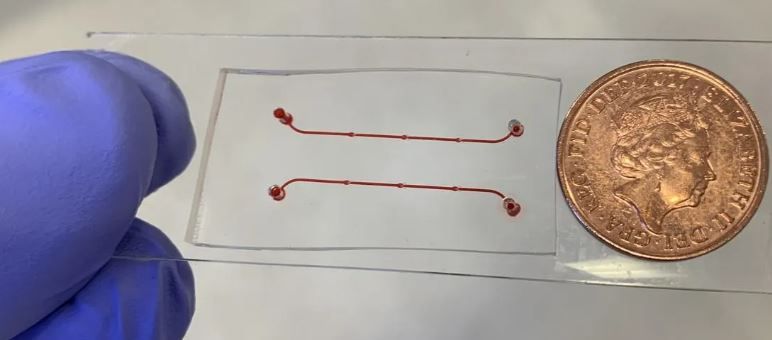
“Our portfolio of gastrointestinal (GI) and respiratory studies will also be able to grow with the addition of new endoscopy equipment. One of the key GI trials to benefit will be the INCEPTION clinic for patients with Inflammatory Bowel Disease (IBD). This trial aims to improve diagnosis and prognosis, and make more informed decisions on IBD treatment through biomarker discovery and implementation, by understanding more about how different microbiomes affect gut and oral immune responses.”
Professor Lorraine Harper, NIHR Birmingham Clinical Research Facility Programme Director, added: “We are tremendously proud that our hospitals have been selected for this award from the NIHR to improve the delivery of research in our local population. The award, which builds on existing clinical-academic collaborations facilitated by Birmingham Health Partners, will benefit our adult and paediatric patients, improving their access to new therapies and treatments, which can potentially be life-changing.”
Dr. Jan Idkowiak, NIHR Birmingham Clinical Research Facility Director (BWC), said: “This is very exciting. This award allows us to expand our ability to deliver cutting-edge clinical research beyond the Children’s Hospital, as it will enable us to include pregnant women and their children at the Women’s Hospital. This will be a huge benefit for our patients and will offer great opportunities to develop new therapies.”
Professor Philip Newsome, Director of the NIHR Birmingham Biomedical Research Centre (BRC), commented: “This is fantastic news for both the CRF and for the organisations that work with them, like the Birmingham BRC. The CRF has been a key partner in delivering many of our experimental research studies, and we collaborate closely on our training, patient and public involvement, and equality, diversity and inclusion programmes too. We are looking forward to continuing working together to deliver patient benefit.”